Blood vessels are the series of tubes that are used to pump blood throughout the body. There are three types of blood vessels: arteries, veins and lymphatics.
Arteries carry oxygen-rich blood away from the heart to every part of the body, including the brain, intestines, kidneys, arms, legs and the heart itself. When disease occurs in the arteries, it is called arterial disease. Veins return blood back to the heart from all parts of the body. When disease occurs in the veins, it is called venous disease. Lymphatics are a third type of blood vessel that return fluid from the skin and other tissues to the veins.
Three of the most recognized vascular diseases include:
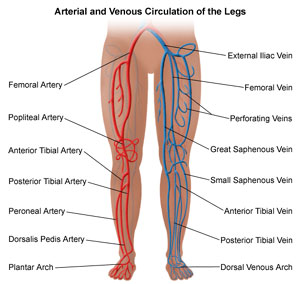
Peripheral vascular disease (PVD) is a slow and progressive circulation disorder. It may involve disease in any of the blood vessels outside of the heart and diseases of the lymph vessels—the arteries, veins, or lymphatic vessels. Organs supplied by these vessels such as the brain, heart, and legs, may not receive adequate blood flow for ordinary function. However, the legs and feet are most commonly affected, thus the name peripheral vascular disease.
Conditions associated with PVD that affect the veins include deep vein thrombosis (DVT), varicose veins, and chronic venous insufficiency. Lymphedema is an example of PVD that affects the lymphatic vessels.
When PVD occurs in the arteries outside the heart, it may be referred to as peripheral arterial disease (PAD). However, the terms "peripheral vascular disease" and "peripheral arterial disease" are often used interchangeably. It's frequently found in people with coronary artery disease, because atherosclerosis, which causes coronary artery disease, is a widespread disease of the arteries.
Conditions associated with PAD may be occlusive (occurs because the artery becomes blocked in some manner) or functional (the artery either constricts due to a spasm or expands). Examples of occlusive PAD include peripheral arterial occlusion and Buerger's disease (thromboangiitis obliterans). Examples of functional PAD include Raynaud's disease, Raynaud's phenomenon, and acrocyanosis.
Venous disease refers to all conditions related to or caused by veins that become diseased or abnormal. Venous disease is quite common -- about 15 percent of the adult population is affected. Mild venous disease is usually not a problem for patients, but as venous disease worsens, it can become crippling chronic venous insufficiency.
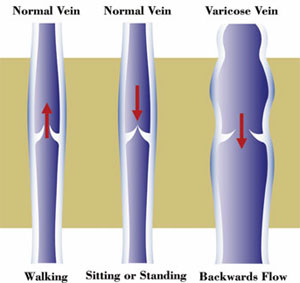
In the normal circulation, arteries carry oxygen rich blood from your heart to the body, and veins return the blood to your heart. Veins have one-way valves along their length to keep the blood flowing to the heart. As muscles contract, the blood is squeezed forward in the veins. When muscles relax, the valves shut to prevent blood from flowing backward.
There are three types of veins in your legs: superficial veins, communicating veins, and deep veins. Superficial veins lie just under the skin and carry about 10 to 15 percent of the blood in your legs. Superficial veins drain into communicating veins, which drain into deep veins. Deep veins lie inside the muscles (remember muscles are responsible for pumping) and carry 85 to 90 percent of the blood back to the heart.
If the vein walls become weak or damaged, or if the valves are stretched or injured, the system stops working normally and the blood begins to flow backward when the muscles relax. This creates unusually high pressure in the veins, resulting in even more stretching, twisting, and swelling of veins. The abnormal veins with their sluggish blood flow create disorders known as venous disease.
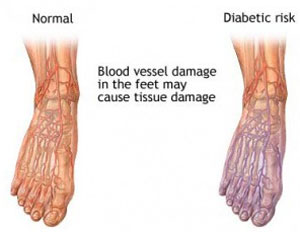
Foot problems are a major reason behind hospitalizations for diabetics. Diabetes can affect nerves in the foot and prevent you from feeling injuries. It can also cause reduced or altered blood flow, which can prevent injuries from healing. Because minor injuries can become major infections among diabetics, it is important to keep a diabetic foot healthy. Prevention is the key to avoiding foot problems in diabetic patients.
The loss of nerve function – neuropathy – among diabetic patients in their feet and legs typically develops over time. Because patients cannot feel foot injuries as acutely as those without diabetes, they may inadvertently ignore foot problems. Therefore, pain is not an early indicator of problems in diabetic patients. Poor circulation and decreased immunity to infection can also lead to serious diabetic foot problems.
Symptoms of diabetic foot problems include pain or a tingling foot sensation in the feet at night. Ulcers, infections, and other problems may be painless. As a result, routine self-inspection of each foot is of utmost importance. Additionally, patients may experience unsteadiness in standing and walking due to the loss of sensation. Finally, the foot may have swelling, redness, ulcers, and bleeding, all of which should alert the patient to call a physician.
Serious foot problems that have resisted conservative treatment methods may require surgery. Surgery may be aimed at removing a foot infection, realigning bony deformities, or an amputation to prevent further problems.
Feel free to contact us
